Simplify prior authorizations: workflow strategies for small and solo practices
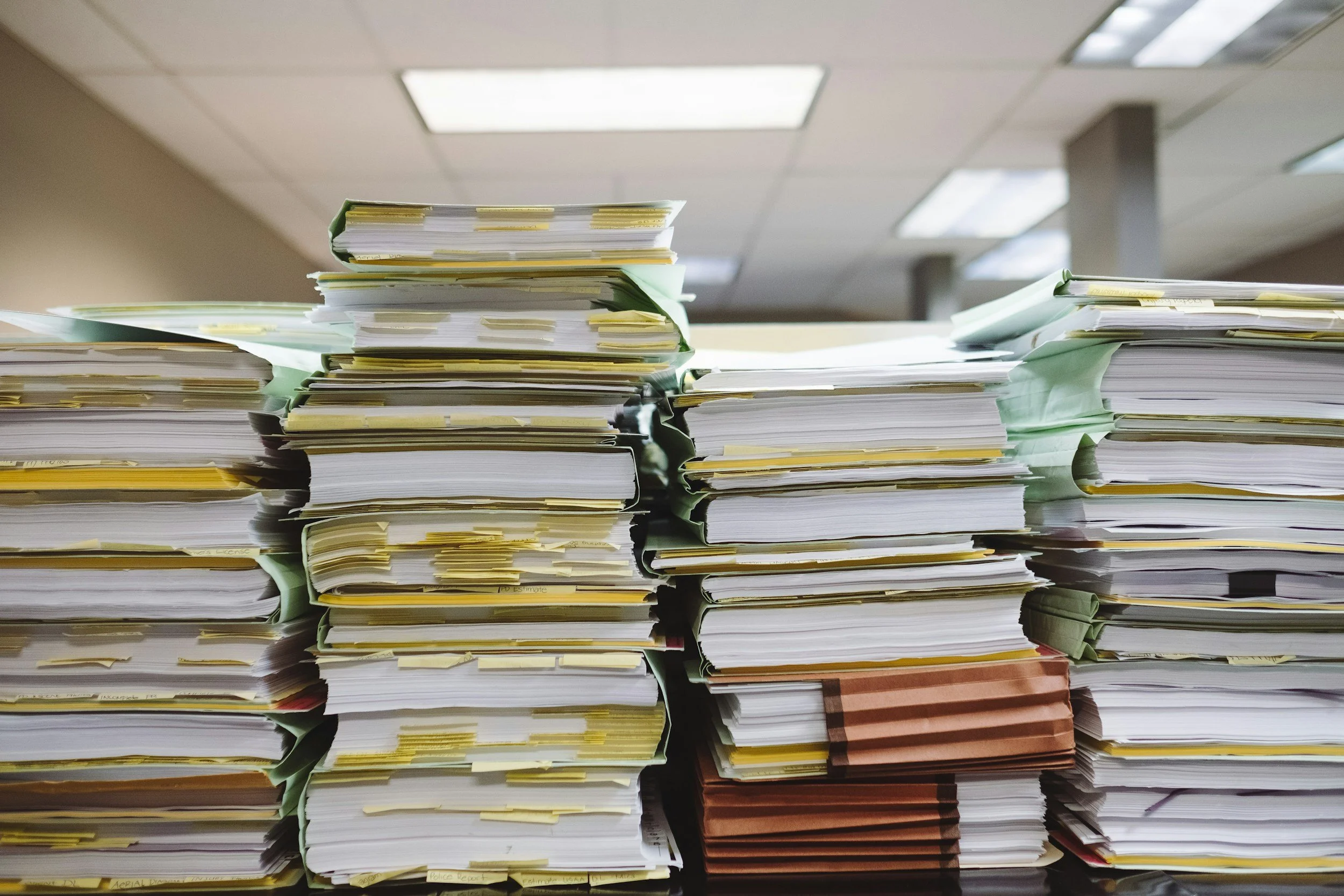
Prior authorizations are one of the most disruptive parts of running a small or solo independent practice. They interrupt your day, delay care, create rework, and generate uncompensated labor. And because you don’t have a large team to absorb the impact, every PA lands directly on your schedule.
You can’t eliminate prior authorizations, but you can make them faster, more predictable, and far less disruptive. The strategies below focus on workflow design, operational clarity, and small steps that reduce the burden without adding complexity.
1. The real cost of prior authorizations
Prior authorizations affect more than just your time. They create:
unpredictable interruptions
delayed care and delayed revenue
documentation burden
back‑and‑forth with pharmacies and payers
cognitive load and context switching
patient confusion and follow‑up messages
For small practices, these costs add up quickly. A few minutes here and there can easily turn into hours of uncompensated work each week.
2. Build a reusable PA packet
Most PAs require the same documents, the same justification language, and the same clinical details. Creating a reusable packet reduces rework and speeds up the process.
Workflow solutions
Create a packet with your most commonly needed documents.
Include templates for justification language.
Add a simple checklist for required elements.
Store everything in a predictable location.
Update the packet quarterly to keep it current.
What you can do this week
Assemble your top three commonly used documents into a single packet.
Add a basic checklist of required elements.
Create a shared folder or shortcut so the packet is easy to access.
3. Create a predictable PA queue
Handling PAs in real time is one of the biggest sources of disruption. A queue allows you to capture requests immediately but process them on your terms.
Workflow solutions
Stop handling PAs as soon as they arrive.
Use a queue to batch PA work.
Set a daily or twice‑daily review time.
Capture requests immediately but complete them later.
Reduce interruptions and context switching.
What you can do this week
Set up a basic PA queue using your EHR, task list, or a simple shared document.
Choose one time per day to process PAs.
Add a “capture, don’t complete” rule to reduce workflow interruptions
4. Identify and reduce high‑friction medications and tests
Some medications and tests trigger PAs far more often than others. Reducing reliance on these options can significantly decrease your PA volume.
Workflow solutions
Review which medications and tests trigger the most PAs.
Identify clinically appropriate alternatives.
Build a quick‑reference list for easy prescribing.
Update prescribing habits to reduce predictable PA volume.
Review payer formularies for preferred options.
What you can do this week
Identify one high‑friction medication that consistently triggers PAs.
Review alternatives that may reduce PA frequency.
Update your prescribing template or quick‑pick list.
5. Use templates to reduce back‑and‑forth
Most PA delays come from missing information or inconsistent justification language. Templates reduce rework and improve approval rates.
Workflow solutions
Create templates for common PA justifications.
Standardize your clinical language for clarity and completeness.
Reduce back‑and‑forth with payers.
Improve approval rates by including required elements upfront.
Use AI to draft or refine justification text.
What you can do this week
Create one justification template for a commonly requested PA.
Add it to your PA packet.
Use AI to refine the language for clarity and completeness
6. Use AI to accelerate documentation and appeals
AI can dramatically reduce the time you spend writing justification letters, summarizing charts, or drafting appeals.
Workflow solutions
Summarize chart notes to extract key clinical details.
Draft justification letters quickly.
Draft appeal letters when needed.
Reduce manual writing time.
Standardize language across PAs.
What you can do this week
Use AI to summarize one complex chart for a PA.
Use AI to draft one justification paragraph.
Save the output as a reusable template.
7. Reduce patient confusion and follow‑up questions
Patients often don’t understand the PA process, which leads to follow‑up messages, frustration, and additional uncompensated work.
Workflow solutions
Create a simple patient‑facing explanation of the PA process.
Set expectations early to reduce follow‑up questions.
Use templates for PA status updates.
Add a “next step” sentence to reduce uncertainty.
Include PA information in your after‑visit summaries.
What you can do this week
Add a PA explanation to your after‑visit summary.
Create a template for PA status updates.
Add a “next step” sentence to reduce patient confusion.
Takeaways
Prior authorizations are disruptive, but they can be made predictable.
Reusable packets reduce rework and speed up the process.
Queues prevent interruptions and protect your schedule.
Templates and AI reduce documentation time and improve approval rates.
Clear patient communication reduces follow‑up messages and confusion.
Let’s build your practice—together
How Inside Out Medicine can help
If prior authorizations are overwhelming your team, Inside Out Medicine can help you build streamlined, specialty‑aligned workflows that save hours each week.
Our resources help you simplify prior authorizations, reduce interruptions, and create more predictable days. If you want support applying these strategies in your own practice, we can help you get there.
See what’s possible for your practice
Talk with us about your goals
Start improving your practice today
About Inside Out Medicine
Inside Out Medicine helps independent medical practices reduce administrative burden, improve efficiency, and strengthen team resilience
Practice operations we improve: Independent medical practice consulting, workflow redesign, prior authorization optimization, digital transformation for clinics, patient experience improvement, medical practice revenue growth, staffing and retention strategies, operational efficiency for healthcare teams.
RECOMMENDED FOR YOU